ROI of Patient Safety Technologies: A Financial Perspective
Don Marcello
The Economic Value of Investing in Patient Safety

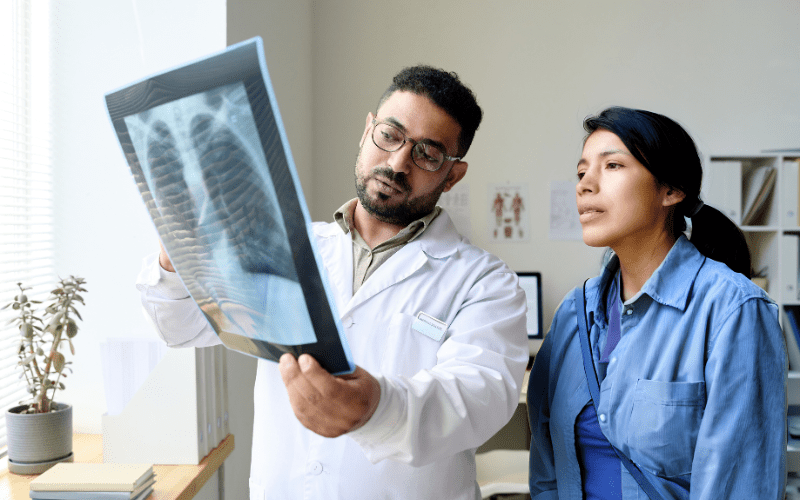
Healthcare facilities face constant pressure to balance quality patient care with financial sustainability. Patient safety technologies yield significant returns in both patient outcomes and financial performance. This article examines the return on investment (ROI) of patient safety technologies, focusing on innovations like the RightSpotpH® Indicator for NG/OG tube placement verification.
Healthcare administrators must evaluate new technologies for both clinical benefits and economic impact. The most successful patient safety can improve care quality while also delivering measurable financial value. For hospital CFOs and financial decision-makers, understanding this dual benefit is essential for proper resource allocation.
The Hidden Costs of NG/OG Tube Misplacement
Nasogastric and orogastric tube misplacements pose serious patient safety concerns with substantial financial implications. When tubes are incorrectly positioned, the consequences include:
- Medical complications requiring extended hospital stays
- Increased treatment costs for arising complications, such as non-ventilator hospital-acquired pneumonia
- Potential liability and litigation expenses
- Higher readmission rates
- Decreased patient satisfaction scores
And those costs don’t stop at treatment—they ripple out across your whole care system.. The Agency for Healthcare Research and Quality estimates preventable medical errors cost the U.S. healthcare system billions annually, with a significant portion attributable to procedural complications like tube misplacements.
A single case of aspiration pneumonia caused by tube misplacement can add $20,000-$40,000 to a patient’s hospital bill. For healthcare systems operating on thin margins, these preventable expenses directly impact the bottom line and diminish resources available for other care priorities.
Quantifying the ROI of the RightSpotpH® Indicator
When evaluating the RightSpotpH® Indicator for your facility, you need clear financial metrics to justify the investment. Our hospital partners consistently report returns in three key areas: direct cost reduction, operational efficiency, and quality improvement incentives. By analyzing these factors in your specific context, you can build a compelling business case for implementation.
Direct Cost Savings
The RightSpotpH® Indicator provides immediate pH verification of tube placement, offering several areas of measurable cost reduction:
Reduced X-ray Usage
Traditional verification methods often rely on X-rays, which incur costs for:
- Equipment usage
- Radiologist interpretation
- Staff time for transport and positioning
- Documentation and reporting
Each avoided X-ray represents a direct cost saving of $200-$400, depending on the facility. The rate of X-ray use for placement confirmation also varies, with perhaps 20–30% of tube placements requiring an X-ray. With the RightSpotpH®, that rate drops to approximately 5%. For a hospital performing hundreds of tube placements monthly, these savings quickly accumulate.
Curious about how this applies to your facility? For hospitals currently using pH strips, or relying on X-rays to verify placement, our ROI Calculator helps estimate your potential cost savings with the RightSpotpH® Indicator.
Decreased Length of Stay
Expedited verification of tube placement allows for:
- Faster initiation of feeding or medication
- Reduced complications from misplacements
- More efficient care protocols
A single day of inpatient care costs an average of $2,500. Even a modest reduction in length of stay for patients requiring NG/OG tubes translates to substantial savings.
Fewer Misplacements, Fewer Costly Complications
The accurate placement verification provided by the RightSpotpH® Indicator helps prevent:
- Aspiration pneumonia (average treatment cost: $20,000+)
- Non-ventilator hospital-acquired pneumonia (NV-HAP)
- ICU admissions due to complications
Indirect Financial Benefits
Beyond direct cost savings, the RightSpotpH® Indicator contributes to financial performance through:
Improved Resource Allocation
Healthcare staff can redirect time from repetitive verification procedures to direct patient care, improving:
- Staff productivity
- Care efficiency
- Patient throughput
Enhanced Reimbursement Potential
Value-based payment models increasingly tie reimbursement to quality metrics that can be positively affected by improved tube placement protocols:
- Reduced 30-day readmission rates
- Decreased hospital-acquired condition incidence
- Improved patient satisfaction scores
Implementation Considerations for Maximum ROI
To maximize financial return on the RightSpotpH® Indicator at your facility, you should:
- Develop clear clinical protocols integrating the technology into your existing workflows
- Track your relevant metrics before and after implementation to quantify your actual savings
- Calculate both direct and indirect cost impacts specific to your facility’s financial structure
- Communicate ROI data to your leadership team and clinical champions
- Use your financial outcomes to inform future safety investments
Your financial and clinical leaders should collaborate to establish baseline measurements before implementation. This provides the comparative data you need to accurately calculate ROI. When you track both clinical outcomes (complication rates, length of stay) and operational metrics (staff time, resource utilization), you create a comprehensive ROI picture that resonates with your stakeholders.
Beyond the Bottom Line: Comprehensive Value
While financial ROI remains important, the comprehensive value of patient safety technologies includes:
- Improved patient outcomes and experiences at your facility
- Enhanced staff satisfaction and retention on your clinical teams
- Strengthened institutional reputation in your healthcare market
- Alignment with safety and quality initiatives your organization has prioritized
These factors contribute to long-term institutional success beyond immediate financial returns. Healthcare systems with strong safety records typically outperform peers on most financial metrics, demonstrating that patient safety and fiscal responsibility are complementary goals.
Fitting RightSpotpH® Into Your Safety Program
The RightSpotpH® Indicator works best when integrated into your broader patient safety strategy. Many facilities incorporate pH testing into their comprehensive tube management protocols, which may include:
- Standardized insertion procedures
- Regular placement verification schedules
- Electronic health record documentation templates
- Staff competency assessments
- Patient education materials
When your staff members understand how the technology fits into their overall workflow, adoption improves and your financial returns increase. Most facilities experience an adoption curve of 3-6 weeks, after which the process becomes routine for clinical teams.
Invest in Patient Safety Technology with Proven ROI
The RightSpotpH® Indicator represents a strategic investment in both patient safety and your facility’s financial performance. By providing rapid, accurate verification of NG/OG tube placement, this technology helps your healthcare facility reduce costs, improve outcomes and allocate resources effectively. The gastric pH testing approach aligns with evidence-based practice while delivering measurable financial benefits for your organization.
Compared to other technologies that rely on electromagnetic tracking or CO2 detection, the RightSpotpH® Indicator offers a more cost-effective solution with fewer technical limitations and simpler implementation. Your facility can typically implement the system within 4-6 weeks, including staff training and protocol development.
Contact Us to Setup a Live Demo to learn how RightBio Metrics can help your facility achieve significant ROI through improved patient safety. During your personalized demo, we’ll review your current verification processes, estimate potential cost savings, and answer specific questions about implementation at your facility.
Frequently Asked Questions
Here are answers to common questions about the financial aspects of implementing the RightSpotpH® Indicator at your healthcare facility:
How quickly can healthcare facilities expect to see ROI from the RightSpotpH® Indicator?
Your facility will likely see observable cost savings within the first quarter of implementation, with full ROI typically achieved within 6-12 months depending on your usage volume and existing verification protocols.
How does the RightSpotpH® Indicator compare to traditional methods in terms of cost-effectiveness?
The RightSpotpH® Indicator offers your facility immediate verification without overly relying on time-consuming and expensive of X-rays. While traditional methods like auscultation may seem less expensive initially, they carry higher costs related to inaccuracy and potential complications that impact your bottom line.
Can smaller healthcare facilities achieve meaningful ROI with this technology?
Yes. If you operate a smaller facility, you’ll often see proportionally similar or greater ROI, as the prevention of even a few complications or extended stays can significantly impact your financial performance.
How is ROI measured when implementing the RightSpotpH® Indicator?
Your ROI calculation should include direct cost savings (reduced X-rays, shorter lengths of stay, fewer complications) and indirect benefits (staff efficiency, time savings, improved reimbursement metrics) compared to implementation and ongoing costs.
Does the RightSpotpH® Indicator require significant staff training that might affect ROI?
The RightSpotpH® Indicator is designed for ease of use with minimal training required for your team. Care givers can learn to use the device within minutes.
How does investing in pH testing for tube verification affect liability insurance costs?
When you implement evidence-based safety technologies like the RightSpotpH® Indicator, your facility may benefit from favorable liability insurance assessments, potentially reducing your premium costs over time. Some risk management programs may recognize standardized verification processes as a factor in liability calculations — check with your provider.
How does the RightSpotpH® Indicator integrate with existing clinical workflows?
The technology is designed to fit into your current tube management processes with minimal disruption. Most facilities incorporate pH testing as a replacement for less reliable verification steps, maintaining the same documentation systems while improving accuracy and efficiency.